November is Diabetes Awareness Month, and as we focus on understanding and addressing the challenges faced by those living with diabetes, it’s crucial to shed light on a lesser-known aspect of the disease—the profound connection between diabetes and skin complications. As a medical professional entrenched in the realms of diabetes management and skin disorders, I often find myself not only navigating the systemic complexities of this metabolic condition but also exploring its unique impact on the body’s largest organ—the skin.
A Global Challenge
As the number of people living with diabetes is constantly growing so is the burden and scope of chronic wounds. With the International Diabetes Federation (IDF) projecting a 50% rise in the disease, reaching 783 million cases by 2045, wounds associated with diabetes are expected to rise as well. This global surge paints a concerning picture, with predictions indicating a rise in chronic, slow-healing, or non-healing diabetic wounds and ulcers. These wounds are more than mere inconveniences – they are potential gateways to severe infections and complications, posing a significant threat to the overall well-being of individuals with diabetes.
The Skin-Deep Connection
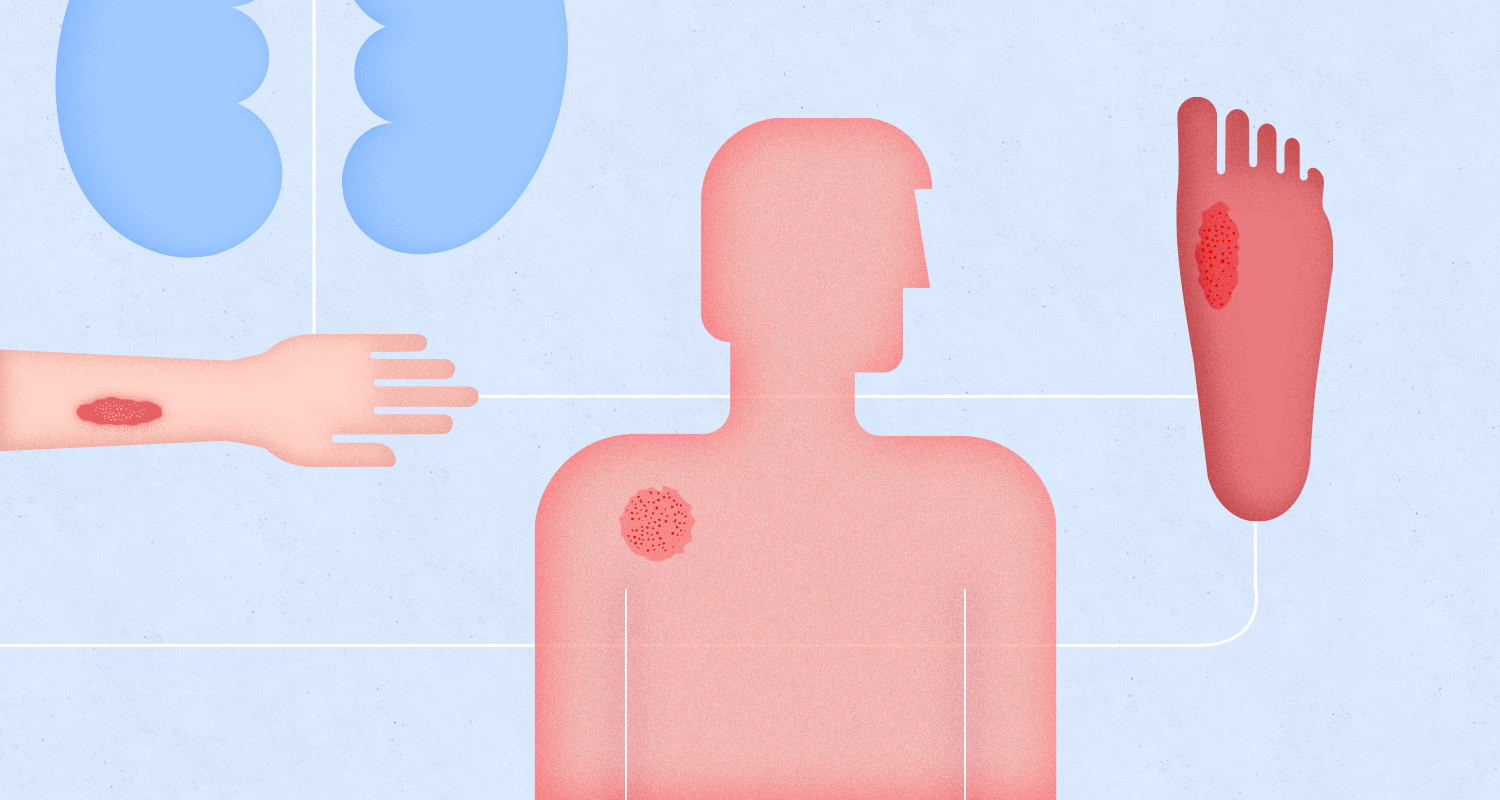
The dynamic relationship between diabetes and various cutaneous manifestations goes beyond cosmetic concerns, offering valuable insights into the broader health of patients. Throughout my clinical rotations in hospitals and primary care settings, I encountered diabetic patients in diverse departments. From managing cellulitis cases in the internal medicine department to addressing diabetic foot ulcers in dermatology, handling more complex cases in vascular surgery, witnessing post-amputation care in orthopedic surgery due to combined vascular and diabetic chronic wounds, and engaging in rehabilitation efforts, the prevalence of these manifestations underscores the necessity for a comprehensive and collaborative approach to diabetic care. Recognizing these dermatologic manifestations early in the course of diabetes enables us, the clinicians, to intervene proactively, potentially influencing patient outcomes and enhancing their overall quality of life.
Diabetes and Wound Healing: A Troubling Tango
Wound healing, a complex physiological process, becomes intricate for those with diabetes, as elevated blood glucose disrupts the coordinated dance between cells, mediators, and growth factors. Persistent high glucose hampers immune function, increasing susceptibility to infections and impeding wound closure. Additionally, diabetes can lead to circulatory issues, delaying nutrient delivery to wounds, while diabetic neuropathy heightens the risk of unnoticed injuries.
For patients living with diabetes, even minor wounds become potential health threats. Without proper management, slow-healing wounds can lead to serious infections, which may spread to nearby tissues and become life-threatening. Untreated infections can escalate to osteomyelitis, a condition where infection spreads to the bone, and in severe cases, it may progress to gangrene—a common cause of amputations in individuals living with diabetes.
Overcoming Wound Care Challenges
The path from diagnosing to effectively treating diabetic ulcers is riddled with challenges in the healthcare system. A significant hurdle is the shortage of wound care nurses, leading to delayed interventions and potential gaps in follow-up care. Adding to the complexity is the reliance on outdated wound measurement practices, such as rulers, introduces subjectivity and limits precision. This discord between traditional methods and evolving healthcare technology compounds challenges for both patients and healthcare professionals
Minuteful for Wound is a digital wound management solution that provides accurate measurement and documentation of chronic wounds using a smartphone and connected portal. It allows for better, more accurate decision-making in the realm of diabetic wound care management, introducing a paradigm shift by providing healthcare professionals with accurate, comprehensive wound data. This solution enables the development of tailored care plans, facilitating timely interventions, and preventing the progression of diabetic wounds.
Minuteful for Wound goes beyond just measurement—it facilitates remote consultations, bridging gaps in care and providing a lifeline for patients in need. In a collaboration with one of our partners, an outpatient engaged with the Minuteful for Wound app. Initially presenting a stable granulating arterial wound, the patient noticed a slight increase in pain, prompting instant image sharing with the clinician through the app. Despite a distant appointment, the clinician detected unexpected deterioration through the Minuteful for Wound portal. Quick response led to an immediate clinic visit, ensuring timely intervention and limb preservation. This case underscores the critical role of remote monitoring platforms like Minuteful for Wound in early detection, facilitating prompt intervention, and ultimately enhancing outcomes in wound care.
A Personal Call to Action
By understanding the profound connection between diabetes and skin complications, we can work towards proactive solutions, easing the burden on both patients and the healthcare system. It’s time to amplify awareness, foster education, and drive research initiatives that pave the way for a brighter, healthier future for individuals living with diabetes.