Treating chronic wounds is both an art and a science. There can be no replacement for the experience of a seasoned wound clinician. But oftentimes the basic question at the heart of wound care—whether or not a wound is healing—is difficult even for an expert to answer objectively.
To make informed decisions, clinicians need reliable and accurate data, but the tools available to most of them are rudimentary. For example, many clinicians use paper rulers to measure wounds, even though the results have been shown to be inaccurate. Visual documentation is a step in the right direction, with the potential to track wounds over time, inform decisions and expedite healing. But when used as the basis for measurements, even the best 2D photography can produce skewed and unreliable results. For photography to serve as an objective source of truth—allowing for measurement, analysis and tracking of wounds over time—it needs an extra dimension.
The Problem with 2D Measurements
Two-dimensional measurements—the measurements produced on the basis of traditional 2D photography—work by comparing the wound to an element with a known size, usually an adhesive sticker placed alongside the wound, that serves as a basis for comparison. But with this method, measurements captured from slightly different camera angles can produce very different results. To determine whether or not a wound is healing, every millimeter is important.
The root of the problem is that 2D imaging assumes that the wound lies on a flat plane and fails to take body curvature into account, leading to inaccurate measurements. Attempting to calculate the wound’s surface area—based on two inaccurate measurements—only compounds the error.
Beyond its inaccurate measurements, 2D imaging also cannot be relied upon for conducting comparisons of wound imagery over time. Comparing images requires that the same camera angle be consistently reproduced between visits. But with clinicians—sometimes different ones every week—operating under time pressure from patients’ homes, there are often errors. Additionally, the reference sticker must be placed on the exact same plane as the wound, which is usually impossible when dealing with some of the most common types of wounds, such as diabetic foot ulcers.
The Reliability and Accuracy of 3D Imaging
3D imaging solves the problems of 2D photography by creating a true-to-life model of the wound that accounts for curvature. This enables accurate area measurements, as well as precise comparisons with earlier and later renderings—meaning that the wound’s progress can be reliably tracked over time.
Instead of one image, 3D imaging works by capturing a series of images. Those images are analyzed using sophisticated photogrammetry techniques to map and reconstruct a full three-dimensional model of the wound—proportions, dimensions and curvature all intact. And because every point on the model has been calculated, 3D imaging allows for standardized measurements that are very difficult to conduct using rulers or 2D measurements. 3D measurements are agnostic to elements that interfere with 2D measurements, such as variance in camera angle, clinician, and location. They also allow for more flexibility in placing the reference stickers—of special importance in complicated wounds.
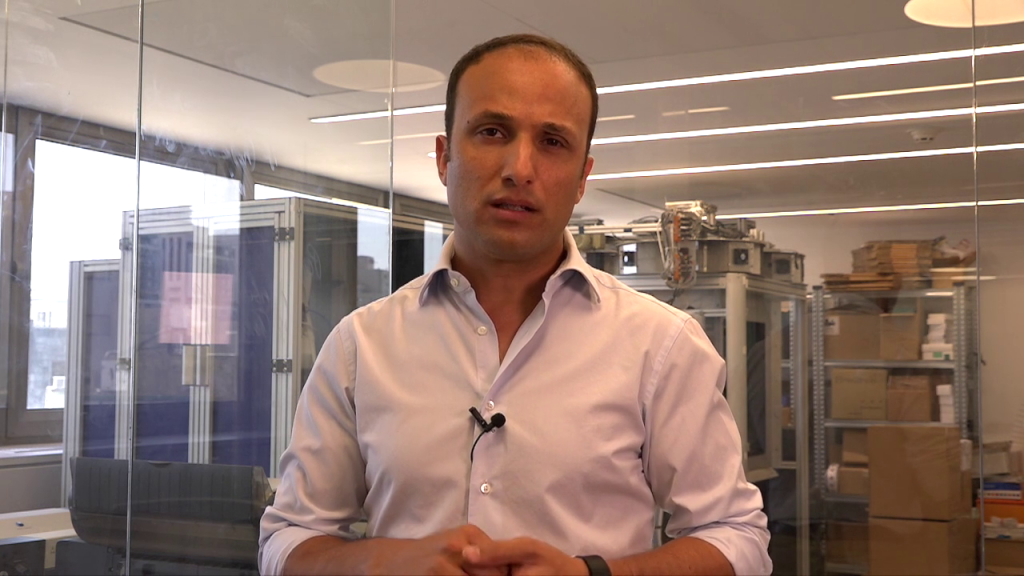
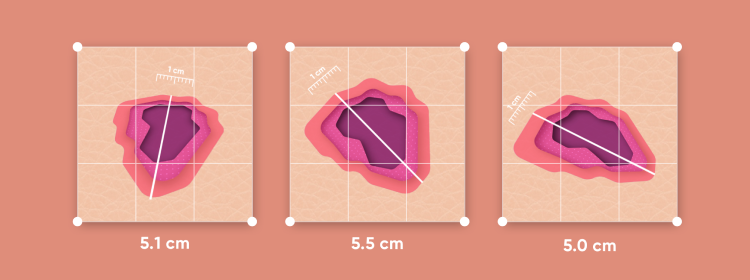
Comparison of Wound Measurement Accuracy Using 3D vs. 2D Imaging
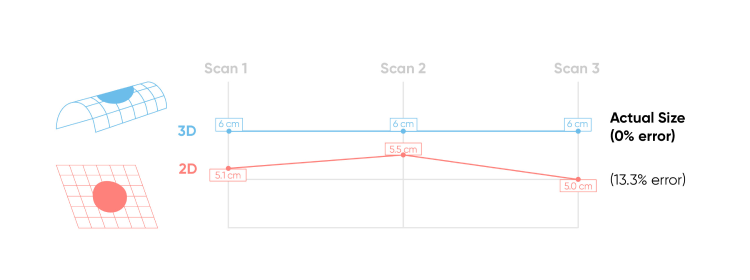
Example based on an internal accuracy study comparing 2D measurements taken with a digital camera and 3D measurements captured with Healthy.io’s smartphone app.
3D measurements consistently deliver more accurate and consistent results than the two-dimension alternative. But the advantages of 3D measurements aren’t abstract or theoretical—they have real-world consequences for the millions of people around the world suffering from chronic wounds, and for the countless nurses and doctors that treat them.
Click here to download a PDF comparing the accuracy of 2D vs. 3D measurements.